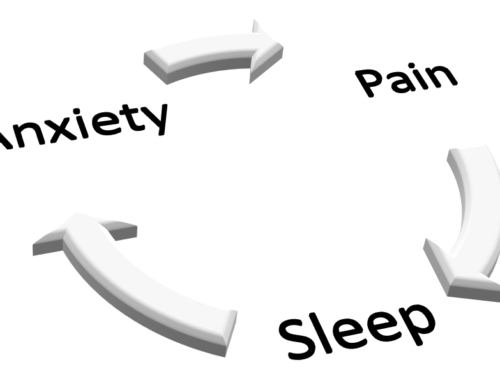
Avoid wrong assumptions that lead to incorrect actions.
When was the last time you made and acted on wrong assumptions? It is so easy to do. You see something from your perspective and your mind fills in the details of the who, what, when, how, and why. It’s often long after you have acted that you are provided with a different perspective that makes the entire situation look different.
A quick, fun example is in this picture. Another proof that I am a geek. I get such a kick out of these pictures. If I believed my eyes I might run in to help the poor guy being lifted into the air.
This happens in healthcare, too. Keep in mind, the provider that is making decisions in the emergency department or the hospital usually knows VERY LITTLE about you. Any information you or a loved one or friend can give is all they have at first.
One day, hopefully soon, these providers will be able to access your medical records and make much more informed decisions. Right now, your doctor has to be contacted then the information sent to the hospital. If it is the weekend or an evening, that can take hours to days. The information then needs to get to your hospital provider from the fax machine or the electronic messaging system. Even then, there might be important information about you that is not even in your doctor’s record.
This leaves those of us making decisions about your care to rely heavily on what we see right now.
I have seen SEVERAL examples in the last few weeks of an older adult reaching medical care confused. The quick wrong assumption has been that the person has dementia. When confused, behaviors often change. A confused person can yell, pull at catheters and IV’s, try to get out of bed, and generally not cooperate. Since the assumption has already been made that dementia is the cause, calming medications are given. These then assure further confusion (but calmer) and make it very hard for the person to get to a point of no confusion.
What can you do to prevent wrong assumptions?
- Carry in your wallet a list of your:
- Allergies
- Medications
- Diagnoses
- Emergency contact information – name, phone number(s)
- If you are accompanying someone to the hospital who is newly confused, explain this to the medical team. Help them understand what this person was like before this event. They need to know the ‘baseline’. If this person was living independently, driving, managing their finances the team needs to know that. If this person was unable to do those things and was getting frequently confused at home, the team needs to know that.
- Share any known history about the current event. If you have been feeling worse and worse for the past three days, make sure they know that. If you have been having pain, explain that including what it feels like, how often you feel it, what makes it better or worse.
- If you have been taking different medications for the past few days, make sure they know that. This often happens when we are in pain or have a cold. We take over-the-counter medications or left-over medications from prior prescriptions. These can cause confusion when mixed with our normal medication regimen.
Speak Up
Again, I have seen several instances in the past few weeks where assumptions are made when someone gets to the emergency department or hospital that make a situation worse.
- In one instance the person’s confusion started as soon as a particular medicine was given. The family member noted that but didn’t speak up. Then medications were added to treat the confused behaviors. We are still trying to taper off of those medications and get this person independent again.
- In another instance, the person had a urinary tract infection. These are famous for making older adults confused. But since no one was there to explain how odd this confusion was for this person, the team assumed this was normal and didn’t find the infection for a while. By then, a couple of medications had been added to treat the confused behaviors. It will take us weeks to taper her back off of these medications.
- In a third instance, the collection of pain medications given after a surgery left the person sleeping most of the day and unable to think clearly. The spouse was dutifully giving the prescribed medicines around the clock. The wrong assumption made here was that this very healthy person over 60 could handle these medications like someone in their 30’s.
- One more instance involved using a medication to treat the side effect of another medication. The second medication (the one used to treat the side effect) is on a list of medicines to avoid in people over 60. Rather than treat the side effect, it made the person nearly unresponsive. In this case, as in several of the others, rather than treat the underlying issue, wrong assumptions were made and actions were taken to treat the symptoms without understanding the back story.
Why ‘Bad Medicine’
Just a side disclaimer. When I was contemplating this blog I saw it as a chance to use the terms, ‘Bad Medicine’. I am a big Bon Jovi fan. I am also a pharmacist. So, I have to admit I love the song, ‘Bad Medicine’.
For more information about how to protect yourself from wrong assumptions leading to bad medicine, contact us at Meds MASH at 410-472-5078 or www.medsmash.com/contact.
For further application, check out my personal blog.